Nursing Team
Radiological Imaging for non-medical referrers
This protocol covers Non-Medical Referrers (NMR) to request imaging for individuals who are aged 16 years and older and are not on a continued care pathway to North Bristol Trust and University Hospitals Bristol & Weston for imaging.
This document and any arrangements made under it apply to registered healthcare professionals, other than medical doctors or dentists, referring patients for imaging with x-rays or radioactive materials employed by General Practice and Primary Care Networks within the BNSSG area (unless indicated under profession specific).
The purpose of this document is to comply with the requirements of the Ionising Radiation (Medical Exposures) Regulations (IRMER) 2017 and its subsequent amendments and revisions, most recently 1st October 2024.

The clinical governance and line management of individual Non-Medical Referrers (NMR) remains with the practices and the Acute Trust Imaging Managers. ALMC and GPCB are happy to offer guidance and advice where appropriate…..
To find out more, please visit here.
Calling all new General Practice Nurses!
The 12-month programme is being run in conjunction with the Avon LMC, BNSSG Training Hub and the BNSSG Integrated Care Board, and is ideal for nurses who are transferring from other specialties (secondary care, community). It includes:
- 4 hours CPD time (pro rota) paid by the training hub.
- A minimum of 1 hour a month of mentoring with a Legacy Nurse (this could involve support with clinics)
- One hour of peer support a month (with other new to practice nurses)
- A N2PP workbook which includes competencies to work through.
- A bespoke programme of training (co-ordinated with the Avon LMC training programme).

Please email legacy.nurses@almc.co.uk for more information.
Revalidation
Revalidation is the process that all nurses and midwives in the UK need to follow to maintain their registration with the NMC, this came into effect from April 2016.
Revalidation is straightforward and will help you as a nurse or midwife demonstrate that you practice safely and effectively. All nurses will have to revalidate every three years to renew their registration.
You will need to submit your application for revalidation online, so it’s very important that you have an NMC Online account. If you haven’t already, you can set up your NMC Online account here.
The NMC also have a microsite which will take you through all the steps to complete.
The Requirements
- 450 practice hours, or 900 if renewing as both a nurse and midwife
- 35 hours of CPD including 20 hours of participatory learning
- Five pieces of practice-related feedback
- Five written reflective accounts
- Reflective discussion
- Health and character declaration
- Professional indemnity arrangement
- Confirmation
Who can act as a confirmer?
It is for individual nurses and midwives to decide who their confirmer should be. However, we recommend that where possible, a line manager should act as the confirmer.
Where this is not possible, there are a number of alternatives. The NMC resources page can help to identify who.
If you need help or advice regarding revalidation, please get in touch with our nursing team at nursing@almc.co.uk.
Our nursing team can also conduct reflective discussions with you, especially if you are a nurse manager who prefers not to engage in this process with a member of your team.
Safeguarding
Safeguarding Children
Guidelines for training requirements for primary care staff are set out in the Intercollegiate Document: Safeguarding Children and Young People: Roles and Competencies for Healthcare Staff. The document sets out the required competencies for staff but also gives recommendations for training which are more complex.
Safeguarding Adults
Information relating to Safeguarding can be found on the BNSSG remedy website. All GPs and primary care staff need to ensure that they have adequate training in safeguarding adults which is appropriate to the role. This is quite a complex area which often causes some confusion. The joint colleges produced and intercollegiate document on the roles and competencies for health care staff which gives definitive guidance.
| Course | Who | Course Length | Course Links | Mandatory or Not |
|---|---|---|---|---|
| Safeguarding Adults – Level 1 | All Practice Staff | Minimum of 2 hours over a 3-year period | e-LfH – Safeguarding Adults – Level 1 | Mandatory: Health Education England |
| Safeguarding Adults – Level 2 | This includes GP reception managers, GP practice safeguarding administrators, GP practice managers, clinic reception managers, healthcare students, health care support workers & phlebotomists. | Minimum of 3-4 hours over a 3-year period | e-LfH- Safeguarding Adults – Level 2 Training, education and learning opportunities should include multi-disciplinary/multi-agency and scenario-based discussion drawing on case studies and lessons from research and audit. | Mandatory: Health Education England |
| Safeguarding Adults – Level 3 | Registered HCP | Minimum of 8 hours over a 3-year period | futurelearn – Safeguarding Adults: Level 3 Training Training, education and learning opportunities should be multidisciplinary and inter-agency. It should be delivered in manner which encourages personal reflection and may include scenario-based discussion, drawing on case studies, serious case reviews, lessons from research and audit. This should be appropriate to the specialty and roles of the participants | Mandatory: Health Education England |
| Safeguarding Children – Level 1 | All practice staff | Minimum of 2 hours over a 3-year period | e-LfH – Safeguarding Children – Level 1 | Mandatory: Health Education England |
| Safeguarding Children – Level 2 | This includes GP reception managers, GP practice safeguarding administrators, GP practice managers, clinic reception managers, healthcare students, health care support workers & phlebotomists | Minimum of 4 hours over a 3-year period | e-LfH – Safeguarding Children – Level 2 Training, education and learning opportunities should also include multidisciplinary and scenario-based discussion. | Mandatory: Health Education England |
| Safeguarding Children – Level 3 | Registered HCP | Minimum of 12 hours over a 3-year period | GPs can request training from BNSSG CCG safeguarding team, please email bnssg.safeguardingadmin@nhs.net for further information. BNSSGCCG – Level 3 Training for Primary Care Staff The BNSSG CCG Safeguarding Team have developed an in-house Level 3 Learning Package, which is detailed and can be used to guide self-directed learning. They recommend this package to all practitioners to build safeguarding knowledge and competences. | Mandatory: Health Education England |
CQC
CQC offer useful information on a range of subjects. Professor Nigel Sparrow OBE, CQC’s Senior National GP Advisor, clears up some common myths about CQC inspections of GP and out-of-hours services and shares agreed guidance of best practice.
A useful example of the myth busters articles is this one on Advanced Nurse Practitioners.
We also have a useful checklist of common questions asked of Nurses when CQC visit.
The Care Certificate
The Care Certificate is a set of standards that social care and health workers stick to in their daily working life.
It is the minimum standards that should be covered as part of induction training of new care workers, this includes HCAs and phlebotomists
For CQC regulated providers, the Care Certificate is expected of care workers joining health and social care since April 2015. The CQC Inspector Briefing that highlights how they look for evidence in their inspections.
Care Certificate supporting resources
If you have any questions or concerns please get in touch with our nursing team at nursing@almc.co.uk.
Advanced Practice
The nurse role has developed within general practice in response to extended clinical and patient demand and workforce issues and have been evolving over the last 20 years. The advanced role is as yet not regulated and tis can cause confusion for nurses, employers and patients. The term ‘Advanced Practice’ defines the level of practice at which the nurse works. Advanced Practitioners are responsible for the safe delivery of a number of defined roles not routinely performed by nurses within primary care, and requires competence in specific areas of knowledge, technical skill, nursing expertise and clinical decision-making.
The RCP /RCN advanced nurse practitioner competencies states that:
“The ANP is an experienced and autonomous registered nurse who has developed and extended their practice skills beyond their previous professional boundaries. The ANP is able to use their expert knowledge and decision making skills, guided by The Code (NMC) in unpredictable situations. This may include managing patients with undiagnosed health care problems and is shaped by the context of their clinical practice”
Department of Health Advanced Practice position statement (2010)
This describes a level of practice, not speciality or role, that should be evident as being beyond that of first level registration.
This focuses on under the following four themes (as agreed by expert practitioners)
- clinical/direct care practice
- leadership and collaborative practice
- improving quality and developing practice
- developing self and others
The expectation is that nurses working at advanced level will have achieved this during extensive clinical/practice experience and following completion of Master’s level education/learning or its equivalent (for example through Master’s level postgraduate certificates/diplomas).
For further advice please contact our nursing team at nursing@almc.co.uk.
Whilst this advice relates specifically to nursing, primary care has seen the development of advanced practitioners from other professional backgrounds in the past few years; notably Pharmacists, Therapists and Paramedics.
Each professional group should look to their own regulatory body for advice.
Nursing Associate
A Nursing Associate is a novel addition to the nursing team, responsible for providing care and support to patients and service users. This role, operational and regulated in England, seeks to fill the skills gap between Health and Care Assistants and Registered Nurses.
Acting as an independent role in its own right, the Nursing Associate also offers a pathway to graduate-level nursing.
Nursing Associates receive training to work with people across all age groups and in various settings. The aim is for this role to allow registered nurses to focus on more complex clinical tasks.
Once qualified and registered, Nursing Associates will deliver care in a range of health and social care settings. Similar to Nurses and other health professionals, they have the opportunity to broaden their scope of practice through further education and experience.
Nurse leaders in England have issued a joint statement emphasising that the role of Nursing Associates is to support, not replace, nurses. They highlight that having a more highly educated and skilled support staff should enable more effective utilisation of graduate nurse resources.
The Nursing and Midwifery Council (NMC) in the UK sets out the standards of proficiency that all nursing associates must meet.
Non-Medical Prescribing
Independent prescribing by Nurses is an established part of General Practice, it has proved that it enhances safe and effective care.
Over the past few years other professional groups have also qualified as independent prescribers further adding value to the Primary Care team.
Our colleagues at Wessex LMC have kindly shared their guidance for non-medical prescribers in general practice.
Treatment Room Checklist
This section provides suggestions for cleaning schedules, emergency equipment, emergency drugs, fridges and cold chain. Please click on the link to view an example spreadsheet of what is required.
Cleaning schedules
As you can imagine the list in the excel spreadsheet isn’t exhaustive and you may need to add or remove items as appropriate to your Practice. Some equipment will not need to be cleaned as regularly and suitable cleaning products should be used, these will be listed in your IC Policy.
Emergency equipment
Practices need to ensure that they have undertaken a risk assessment to decide what equipment they have available and how this is maintained. They will also need to demonstrate:
- staff have been trained in its use
- it is stored safely but easily accessible
- checked (and recorded) on a regular basis and after use
The guidance below relates to Regulation 12 ‘Providers must make sure that the premises and any equipment used is safe and where applicable, available in sufficient quantities’
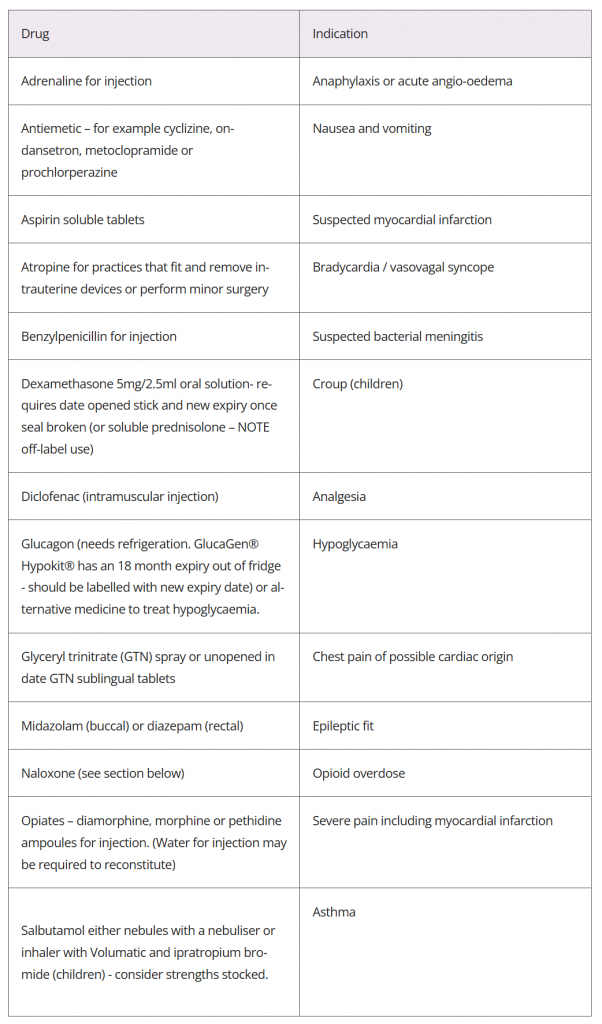
Emergency drugs
There is no definitive answer on what emergency drugs should be available. Practices need to ensure that GPs/Nurses have the training, knowledge and skills to manage emergencies. The list of emergency drugs on the spreadsheet is not “exhaustive and/or mandatory” contents and or omissions would however need to be justified.
Guidance relating to this can be found here, including bags used for home visits.
Fridges
Here is a short list of what to be aware of:
- Vaccines should be stored in a special vaccine fridge and is only used for the storage of vaccines.
- Temperatures should be maintained between 2-8 degrees, minimum, maximum and actual temperature should be recorded daily. It is advisable to have a 2nd thermometer data logger to improve accuracy.
- Remember the 4R’s – Read, Record, Reset & React
- Ideally the vaccine fridge should have its own supply of electricity and or the socket should be clearly labelled to ensure it is not removed or turned off in error.
- The fridge should have a good circulation of air around it and not be placed in a room where internal or external factors can affect the temperature.
- Vaccines should be kept in their original packaging and stored away from the walls and or roof of the fridge. The fridge should not be over full.
- Where possible child immunisation and travel vaccines should be stored separately.
- Vaccines should be rotated and not too much stock ordered at any one time.
- The fridge should be locked when not in use and only accessible to practice staff.
Public Health England (PHE) have published guidance regarding ordering, storing and handling vaccines.
Cold chain
All staff involved in the ordering, delivery and administering of vaccines should be fully aware of the importance of the cold chain and have received training.
Only cool boxes specifically designed to transport vaccines should be used.
All staff should be aware of what to do if there has been a break in the cold chain and this should be recorded as a significant event.
Further guidance can be found here: